Artificial intelligence (AI) tools are becoming a common occurrence in everyday healthcare, especially in the areas of early detection and diagnosis. As lung diseases and the current COVID-19 pandemic become more prevalent around the world, early detection and diagnosis can be literal lifesavers. AI, along with collaborative efforts of the radiological, healthcare industry, and academic communities, are helping to make great strides in the fight against lung disease. Dr. med. Sebastian Schmidt, who works in the area of clinical applications of computed tomography, spoke with us about how AI is being used throughout the process of detection and treatment of lung disease, the new publicly available research algorithm (“CT pneumonia analysis”) from Siemens Healthineers that aims to improve lung screening, and the Open Source Imaging Consortium, a co-operative effort to fight Interstitial Lung Disease.
How can AI help to improve the early detection of lung cancer?
a. How present are AI tools throughout the entire process of detection and treatment?
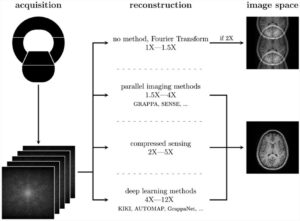
AI tools are well-established to identify nodules in the lung during lung cancer screening CT scans, and for finding incidental lung nodules in CT scans performed for other indications. These tools have been on the market for several years and have proven their utility in clinical practice providing high detection rates, demonstrating their ability to lower the workload of the radiologists and improve quality (Liang et al., 2016).
Increasingly, AI now also guides the CT scanning process: Automated tools define and propose the optimal scan protocol for each patient, thereby ensuring appropriate image quality at the lowest possible radiation dose and reducing unwanted variations and user errors.
Beyond these already established applications of AI, there are many promising developments on the horizon: AI may help to identify the right patients for lung cancer screening. Better selection tools would be beneficial, as with the current guidelines, almost two-thirds of the lung cancers eligible for screening occur outside the eligibility criteria. Therefore, better tools for identification of persons at risk are required and will further improve the screening programs, as the success of lung screening strongly depends on the optimal selection of the participants.
Another area of promising research is the avoidance of unnecessary follow-up examinations: The rate is already in the lower single-digit percent range (Crosbie et al., 2019) if the most recent guidelines are followed. And if more information is included in the assessment there may be further improvement potential. For example, inclusion of texture or radiomics data may help to identify the optimal follow-up regimen for the patient and thereby avoid unnecessary costs and discomfort (Digumarthy et al., 2019).
All these solutions have shown their potential in smaller case series, however, to allow introduction into clinical practice and routine use, more and prospective studies on the safety and efficacy of these methods will be needed.
b. Does the use of AI end at early detection or are there applications for AI tools in the monitoring and follow-up post-diagnosis?
The use of AI tools does not end with diagnosis but will accompany the whole clinical pathway of the patient. Examples are data collection and presentation (e.g. natural language processing of previous reports) treatment selection (systemic therapy, ablation, radiotherapy of surgery), treatment planning (e.g. AI-based organ contouring in radiotherapy) and execution (e.g. surgical navigation systems).
With the increasing number of treatment options and personalization of therapies, the complexity of treatment decisions grows exponentially. This will require new approaches to help the physician to navigate through the growing space of treatment options, which will involve more and more AI tools.
On LinkedIn, we noticed several posts about the new algorithm that SHS made available for everyone. What is the aim of Siemens Healthineers in this regard and how is it received by the customers?
In the last months, we have developed our research algorithm “CT pneumonia analysis” [1] together with radiologists all over the world, and we will now continue the work to translate it into a regulatory cleared product. We have received good feedback from our customers, especially as we were able to give many of them immediate access to the research algorithm and incorporate their feedback. This collaborative approach allowed the team to complete the development of a medical software offering, which normally takes years from idea to regulatory approval, within just a few months. We would like to use this opportunity to thank the global radiological community which supported this development in an unprecedented way (Chaganti et al., 2020).
With the CT pneumonia analysis we aim to provide our customers with new possibilities within our AI-Rad Companion solution, the application is designed to run different algorithms on the same scan and provide all the findings in a report to radiologists and clinicians.
The AI-Rad Companion Chest CT allows comprehensive detection of typical findings in a chest CT:
- Mark and measure lung nodules
- Indicate the presence of coronary calcifications
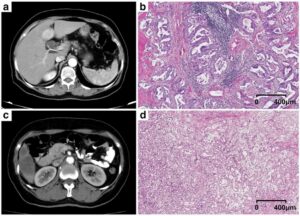
- Mark areas of lung tissue with an elevated tissue density, to identify the infiltrates and consolidations from COVID-19 [2]
- Mark areas of decreased lung density as a sign for Emphysema/COPD
- Perform segmentation and measurement of the heart
- Perform segmentation and measurement of the thoracic aorta
- Measure the height and density of the thoracic vertebra as a sign for osteoporosis and any resulting compression fracture
That means, for instance, that patients who come for a lung cancer screening CT will automatically also have an analysis of other findings in the chest area, including signs of COVID-19. Or, if a patient is scanned for suspected COVID-19, incidental lung nodules are automatically detected and measured. This could have a strong positive impact on the workload of radiologists and of course improve patient outcomes. The algorithm is planned to become part of our AI-Rad Companion Chest CT in countries where the AI-Rad Companion is available.
We strongly believe that using AI for chest CTs requires a holistic approach – a patient with suspected COVID-19 may have lung nodules, an aneurysm, COPD or cardiac conditions requiring early diagnosis and intervention. Any AI tool that only addresses COVID-19 may miss these, especially in a challenging acute care setting, and acute disease may mask non-acute, but nevertheless life-threatening diseases.
We also notice a growing number of case reports of incidentally discovered COVID-19 in chest CT scans for other indication, e.g. oncological examinations. These also require a quick reaction to protect the patient and the surrounding environment – this is a perfect application for AI tools, which can analyze all images immediately and without variation in performance. This enables the radiologist to focus on what really matters: Making the diagnosis and initiating the appropriate actions.
What is the Open Source Imaging Consortium (OSIC) and how do you envision it evolving and changing the game in relation to fighting interstitial lung disease?
The Open Source Imaging Consortium (https://www.osicild.org/) is a co-operative effort between academia, industry and philanthropy to advance the fight against Interstitial Lung Diseases. Here, small and large enterprises from different industries (Imaging, IT and Pharma) and academic institutions from different specialties (pulmonology, radiology and computer science) formed a non-profit alliance to address this significant global health issue.
We believe that the consortium approach is perfect for this rare, but highly complex group of diseases, with its high morbidity and mortality. Single centres will always be challenged to gather sufficient patient numbers and experience on their own, and it requires a multi-centre and multi-disciplinary approach to really improve the outcomes of these patients.
Additionally, ILDs are an ideal field for the application of artificial intelligence: An AI tool can be trained with datasets from tens of thousands of patients and make this combined experience available to any physician in the world, while any individual physician will see much smaller patient numbers of rare diseases, even in the biggest institutions. So, AI is able to combine the experience of a significant number of leading experts in the field and make it available to all physicians and patients worldwide.
a. What is the role that Siemens Healthineers will play as a co-founder of OSIC?
Siemens Healthineer’s role is, beyond financial support, to provide access to state-of-the-art technology, support with know-how and experience. The results of the consortium will be available to the clinical community in an open-source model, and we plan to make these tools available to our large and global customer base in hospitals and imaging centres.
Gain insights about the digital transformation of radiology and how data-driven solutions like AI-powered technologies are helping provide better outcomes and improve patient care.
[1] For research purpose only. Not for clinical use. Safety and effectiveness of the prototype have not been assessed and it is not yet commercially available. Its future availability cannot be ensured.
[2] The Pulmonary Density feature is new in VA12A without FDA Clearance. According to FDA policy “Enforcement Policy for Imaging Systems During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency” issued in April 2020, the manufacturer is allowed to market this feature without FDA-clearance. This policy is intended to remain in effect only for the duration of the public health emergency related to COVID-19 declared by the HHS, including any renewals made by the HHS Secretary in accordance with section 319(a)(2) of the Public Health Services Act (42 U.S.C. 247d(a)(2)).
Pulmonary Density results are not indicated for the diagnosis of COVID-19. Only in vitro diagnostic testing is currently the definitive method to diagnose COVID-19.
Chaganti, S., Balachandran, A., Chabin, G., Cohen, S., Flohr, T., Georgescu, B., . . . Comaniciu, D. (2020). Quantification of Tomographic Patterns associated with COVID-19 from Chest CT. ArXiv.
Crosbie, P. A., Balata, H., Evison, M., Atack, M., Bayliss-Brideaux, V., Colligan, D., . . . Booton, R. (2019). Second round results from the Manchester ‘Lung Health Check’ community-based targeted lung cancer screening pilot. Thorax, 74(7), 700-704. doi:10.1136/thoraxjnl-2018-212547
Digumarthy, S. R., Padole, A. M., Rastogi, S., Price, M., Mooradian, M. J., Sequist, L. V., & Kalra, M. K. (2019). Predicting malignant potential of subsolid nodules: can radiomics preempt longitudinal follow up CT? Cancer Imaging, 19(1), 36. doi:10.1186/s40644-019-0223-7
Liang, M., Tang, W., Xu, D. M., Jirapatnakul, A. C., Reeves, A. P., Henschke, C. I., & Yankelevitz, D. (2016). Low-Dose CT Screening for Lung Cancer: Computer-aided Detection of Missed Lung Cancers. Radiology, 150063. doi:10.1148/radiol.2016150063
 Dr. med. Sebastian Schmidt studied human medicine at the Universities of Berlin and Freiburg, Germany. After working as a resident in radiology, he changed to industry and is currently responsible for medical affairs in the computed tomography business line of Siemens Healthineers. In this role, he works on establishing new clinical applications of Computed Tomography with high patient benefit, like lung cancer screening.
Dr. med. Sebastian Schmidt studied human medicine at the Universities of Berlin and Freiburg, Germany. After working as a resident in radiology, he changed to industry and is currently responsible for medical affairs in the computed tomography business line of Siemens Healthineers. In this role, he works on establishing new clinical applications of Computed Tomography with high patient benefit, like lung cancer screening.